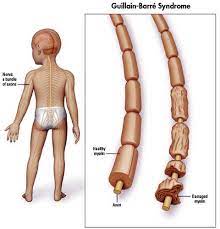
As a doctor, I have witnessed countless medical miracles and shared in the joy of many child survival stories. However, one particular case that stands out in my memory is that of a child with Guillain-Barre Syndrome. This is a rare neurological disorder in which the body's immune system mistakenly attacks the nerves, causing muscle weakness and paralysis.
I first encountered little Janki when she was brought to the hospital with complaints of tingling and numbness in her feet and legs. She was only six years old and had been previously healthy, so her sudden onset of symptoms was deeply concerning. After a thorough examination and NCV study, it became evident that she was suffering from Guillain-Barre Syndrome.
I immediately started Janki on treatment in form of IV IG injection. The goal was twofold: to prevent further nerve damage and to provide supportive care to manage her symptoms. However, it was also essential to monitor her closely for any signs of respiratory distress, as this condition can lead to muscle weakness, making breathing difficult.
Over the course of a few days, Janki’s condition rapidly deteriorated. She started experiencing difficulty breathing and required a ventilator to assist her respiratory function. It was heart-wrenching to witness this sweet little girl's struggle, but we did not lose hope. She required to tracheostomy because of prolonged ventilation.
With intensive care, including physiotherapy to improve muscle strength and prevent joint contractures, Janki slowly started to show signs of improvement. Bit by bit, she regained movement in her limbs, and her breathing became less laboured. As Janki's doctor, I closely monitored her progress and provided on-going support to her family. The road to recovery was long and challenging, with many ups and downs. There were moments of frustration and despair, but also moments of sheer joy as she achieved small milestones.
Finally, after seven weeks, Janki took her first steps. It was an emotional moment for everyone involved. She had overcome immense physical and emotional obstacles, and her strength was truly inspiring. From that point on, she continued to make steady progress, gradually regaining her independence and eventually being discharged from the hospital.
Janki's survival story represents the power of medical intervention, dedication, and the unwavering human spirit. As a doctor, it is moments like these that reaffirm my passion for medicine and remind me that sometimes, even in the face of seemingly insurmountable odds, miracles can happen.
Janki and her family will always hold a special place in my heart. Witnessing her journey from paralysis to walking again was a privilege and an honor. It is a reminder that even in the face of rare and devastating conditions, there is always hopes for recovery.
As a doctor working in the field of trauma medicine, I have witnessed numerous cases of polytrauma, where children are involved in devastating accidents. However, there is one survival story that stands out among all the others, as it highlights the incredible strength and resilience of a young patient.
It was a sunny afternoon when an ambulance rushed into our trauma center, sirens blaring, carrying a seven-year-old girl Vedika ,who had been involved in a severe car accident. The scene was chaotic, with paramedics frantically relaying information about the child's injuries and vitals.
Upon initial assessment, it was evident that she had suffered life-threatening injuries. Her body was covered in bruises and lacerations, and her vital signs were unstable. Her parents, who had also been in the car, were emotionally distraught, but their anxiety soon turned into hope as our team sprang into action.
Within minutes, the paediatric trauma team assembled, consisting of Paediatrician, surgeons, nurses, anesthesiologists, all prepared to tackle the challenges that lay ahead. Every second mattered and maintaining clear communication was crucial in ensuring the best outcome for our young patient.
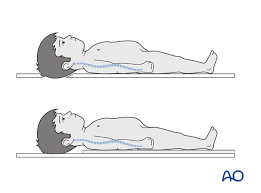
The initial evaluation revealed multiple fractures in her limbs, a severe head injury, and internal bleeding. Our team immediately mobilized to stabilize her condition while ordering a battery of tests to fully understand the extent of her injuries. CT head and chest-abdomen confirm large hematoma in brain with multiple rib fracture with liver laceration. The sheer complexity of her condition was daunting, but we were determined not to let it deter us.
Over the course of the next few hours, our paediatric surgeons skilfully repaired her fractures, while neurosurgeon performed Craniotomy and relived intracranial pressure. For for Liver laceration Blood support with conservative approach was chooses. It felt like a constant battle against time, but we never gave up. The teamwork and relentless dedication of every member of the trauma team were truly remarkable to witness.
Days turned into weeks, and the little girl began showing signs of improvement, little by little. Her pain became more manageable, her movements more purposeful, and her cognitive function slowly started to return. It was an emotional rollercoaster for her parents, as they witnessed their child fight for her life and gradually make a remarkable recovery.
Months of extensive rehabilitation followed, as our patient worked tirelessly to regain her strength, coordination, and speech. It was truly awe-inspiring to see her determined and unwavering spirit despite the immense challenges she faced. Every small achievement was a cause for celebration, not just for her but for the entire medical team that had cared for her.
Today, years later, that little girl is a vibrant teenager, living a fulfilling life. She visits our PICU occasionally, a constant reminder of the tremendous impact we can make as healthcare professionals. Her story has become an inspiration to countless others who are battling their own traumas.As a doctor, it is moments like these that make every long hour, every sleepless night, and every emotionally draining day worthwhile. The survival of this polytrauma child has not only reaffirmed my commitment to saving lives but has also taught me the power of resilience, the
Strength of human spirit and the indomitable will to overcome adversity.

As a doctor, I have encountered countless medical emergencies throughout my career. However, one particular case of diabetes ketoacidosis (DKA) stands out as a remarkable survival story that still gives me hope and affirmation for the power of modern medicine.
It was a regular day at the hospital when , a 11-year old Parv with a known history of type 1 diabetes, was rushed into the emergency department in an unconscious state. His shallow breathing and the sweet smell of his breath immediately alerted the medical team to the possibility of DKA. Without wasting a moment, we swiftly initiated emergency protocol.
The initial blood tests confirmed our suspicion: Parv’s blood sugar levels were alarmingly high, and his blood pH indicated severe acidosis. His body was effectively breaking down fat for energy due to an absolute lack of insulin, which resulted in ketones flooding his bloodstream. We knew that if we didn't act quickly, Parv's condition could rapidly deteriorate into a life-threatening state.
Our first priority was to stabilizeParv’s breathing and acid-base balance. We administered intravenous fluids and electrolytes, adjusting the infusion rate based on the constant monitoring of his vitals. We also provided him insulin therapy, as the primary goal was to suppress ketogenesis and normalize blood sugar levels. It was crucial to strike a delicate balance, as rapid correction could lead to brain swelling or subsequent hypoglycemia.
Over the next few hours, we attentively monitored Parv's response to treatment. Gradually, his breathing became less shallow, and his acidosis improved. However, we were still concerned about potential complications such as cerebral edema, organ dysfunction, or electrolyte imbalances. To ensure his safety, we continued close observation and adjusted our interventions accordingly.
As the hours turned into days, Parv’s gradually regained consciousness and his vital signs stabilized. We carefully introduced a controlled diet to aid his recovery while closely monitoring his blood sugar levels. Our interdisciplinary team worked relentlessly to address all aspects of his care, including nutrition counselling, diabetes management education, and psychological support.
After a week of intensive care, Parv was deemed stable enough to be transferred to a general ward. His recovery was a testament to the dedication of the medical team, as well as Parv's determination to regain control of his health. The case not only highlighted the importance of early recognition and intervention, but also the significance of on-going support for individuals with chronic illnesses like diabetes.
Parv's survival story served as a powerful reminder that DKA, although a severe and potentially fatal condition can be overcome with timely and appropriate medical intervention. As a doctor, cases like Parv's fuel my passion for providing the highest level of care to every patient, no matter how challenging the circumstances. It also reinforces the importance of continuous research and education to improve outcomes and save more lives.
As a doctor, I have seen my fair share of patients battling severe pneumonia, but there is one child's story that will forever stay with me.
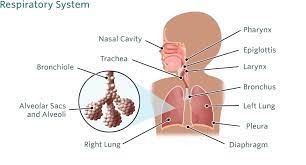
It was a cold winter day when the parents rushed their six-year-old son, Mohamad Rehan, into the emergency room. Mohamad Rehan was struggling to breathe, his tiny chest heaving with every effort, and his face pale and frightened. As I assessed his condition, there was no doubt in my mind that Mohamad Rehanwas in a critical state.
We wasted no time in initiating immediate treatment. Oxygen was administered, and intravenous antibiotics were swiftly started to target the bacterial infection causing his pneumonia. Mohamad Rehan's parents stood by his side, their eyes filled with a mixture of fear and hope. They trusted us to save their beloved child.
For the next few days, Mohamad Rehan’s condition remained touch-and-go. His body fought tirelessly against the infection, but it seemed the pneumonia had taken a strong hold. As doctors, our team worked around the clock, monitoring his vitals, adjusting medications, and praying for a breakthrough.
Despite our efforts, Mohamad Rehan's health kept deteriorating. His lungs were struggling to provide him with enough oxygen, and we had to place him on a ventilator. It broke our hearts to see him in such a vulnerable state, hooked up to machines to help him breathe.
As time passed, we started to doubt if Mohamad Rehan would make it. We prepared his parents for the worst, explaining the gravity of his situation and the uncertain outcome. They clung to hope and drew strength from each other's support.
But then, something remarkable happened. Slowly, ever so slowly, Mohmad Rehan’s condition began to improve. His body responded to the antibiotics and the support of the ventilator, and his oxygen levels started to stabilize. It was a glimmer of hope we desperately needed.
Days turned into weeks, and his progress continued. He was finally able to come off the ventilator, his breathing becoming more rhythmic and steady. He opened his eyes, and a faint smile formed on his pale face. It was as if the strength of his young spirit had triumphed over the shadow of death.
Mohamad Rehan's recovery was slow but steady. We moved him out of the intensive care unit and into a regular hospital room. He was finally able to sit up, eat regular food, and even play with the toys brought to him by the hospital's kind-hearted volunteers. The once somber room was now filled with laughter and hope.
When the day finally came for Mohamad Rehan to leave the hospital, it was an emotional moment for all of us. His parents, overjoyed and tearful, expressed their gratitude for our unwavering dedication. We had witnessed Mohamad Rehan's fight for survival, but it was his resilience, combined with the care and expertise of the medical team, that made his recovery possible.
Seeing Mohamad Rehan walk out of the hospital that day reaffirmed why I became a doctor. It is moments like these that remind us of the profound impact we can have on people's lives.Mohamad Rehan's story will forever remain etched in my memory as a testament to the power of hope, perseverance, and the indomitable strength of the human spirit.